Search
- Page Path
- HOME > Search
Original Article
- Diabetes, Obesity and Metabolism
- Effect of the Concomitant Use of Subcutaneous Basal Insulin and Intravenous Insulin Infusion in the Treatment of Severe Hyperglycemic Patients
- Yejee Lim, Jung Hun Ohn, Joo Jeong, Jiwon Ryu, Sun-wook Kim, Jae Ho Cho, Hee-Sun Park, Hye Won Kim, Jongchan Lee, Eun Sun Kim, Nak-Hyun Kim, You Hwan Jo, Hak Chul Jang
- Endocrinol Metab. 2022;37(3):444-454. Published online June 3, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1341
- 59,133 View
- 241 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
No consensus exists regarding the early use of subcutaneous (SC) basal insulin facilitating the transition from continuous intravenous insulin infusion (CIII) to multiple SC insulin injections in patients with severe hyperglycemia other than diabetic ketoacidosis. This study evaluated the effect of early co-administration of SC basal insulin with CIII on glucose control in patients with severe hyperglycemia.
Methods
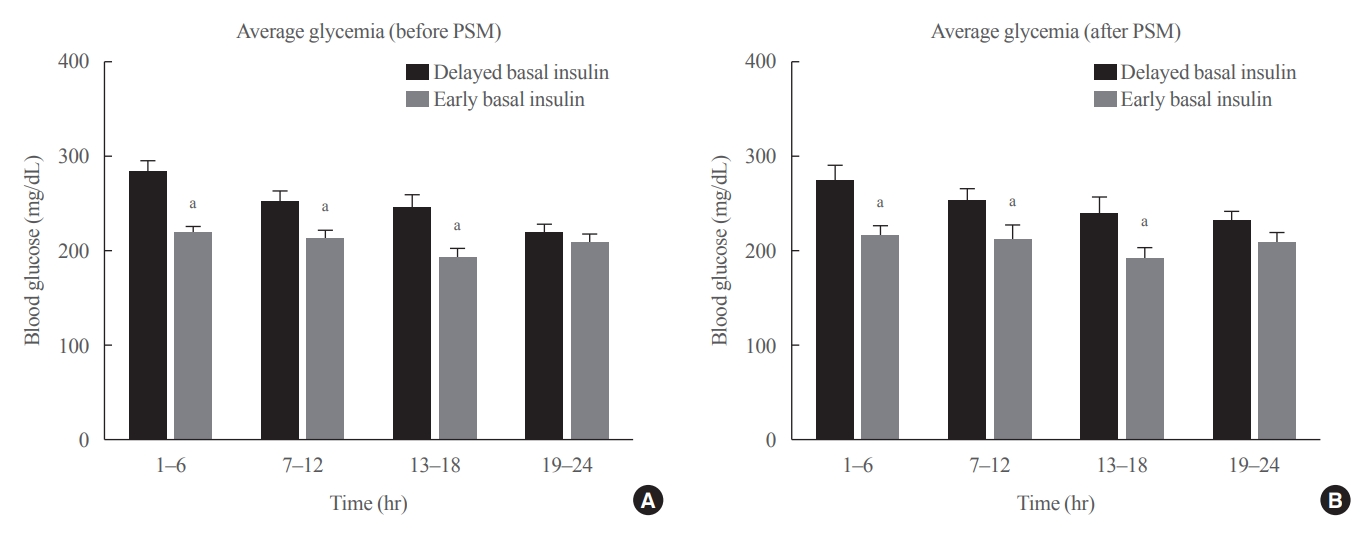
Patients who received CIII for the management of severe hyperglycemia were divided into two groups: the early basal insulin group (n=86) if they received the first SC basal insulin 0.25 U/kg body weight within 24 hours of CIII initiation and ≥4 hours before discontinuation, and the delayed basal insulin group (n=79) if they were not classified as the early basal insulin group. Rebound hyperglycemia was defined as blood glucose level of >250 mg/dL in 24 hours following CIII discontinuation. Propensity score matching (PSM) methods were additionally employed for adjusting the confounding factors (n=108).
Results
The rebound hyperglycemia incidence was significantly lower in the early basal insulin group than in the delayed basal insulin group (54.7% vs. 86.1%), despite using PSM methods (51.9%, 85.2%). The length of hospital stay was shorter in the early basal insulin group than in the delayed basal insulin group (8.5 days vs. 9.6 days, P=0.027). The hypoglycemia incidence did not differ between the groups.
Conclusion
Early co-administration of basal insulin with CIII prevents rebound hyperglycemia and shorten hospital stay without increasing the hypoglycemic events in patients with severe hyperglycemia. -
Citations
Citations to this article as recorded by- 16. Diabetes Care in the Hospital: Standards of Care in Diabetes—2024
Nuha A. ElSayed, Grazia Aleppo, Raveendhara R. Bannuru, Dennis Bruemmer, Billy S. Collins, Laya Ekhlaspour, Rodolfo J. Galindo, Marisa E. Hilliard, Eric L. Johnson, Kamlesh Khunti, Ildiko Lingvay, Glenn Matfin, Rozalina G. McCoy, Mary Lou Perry, Scott J.
Diabetes Care.2024; 47(Supplement): S295. CrossRef - 16. Diabetes Care in the Hospital: Standards of Care in Diabetes—2023
Nuha A. ElSayed, Grazia Aleppo, Vanita R. Aroda, Raveendhara R. Bannuru, Florence M. Brown, Dennis Bruemmer, Billy S. Collins, Marisa E. Hilliard, Diana Isaacs, Eric L. Johnson, Scott Kahan, Kamlesh Khunti, Jose Leon, Sarah K. Lyons, Mary Lou Perry, Priya
Diabetes Care.2023; 46(Supplement): S267. CrossRef - Effectiveness and safety of early insulin glargine administration in combination with continuous intravenous insulin infusion in the management of diabetic ketoacidosis: A randomized controlled trial
Kitti Thammakosol, Chutintorn Sriphrapradang
Diabetes, Obesity and Metabolism.2023; 25(3): 815. CrossRef
- 16. Diabetes Care in the Hospital: Standards of Care in Diabetes—2024

Case Reports
- A Case of Primary Adrenal Insufficiency in a Patient with Acquired Immunodeficiency Syndrome.
- Jae Ho Choi, Suk Chon, Yu Chul Hwang, Jun Seong Son, Seung Joon Oh, Kyu Jeung Ahn, Ho Yeon Chung, Jeong Taek Woo, Sung Woon Kim, Jin Woo Kim, Young Seol Kim, In Kyung Jeong
- Endocrinol Metab. 2011;26(3):253-257. Published online September 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.3.253
- 2,139 View
- 24 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - The adrenal gland is the most commonly involved endocrine organ in patients infected with the human immunodeficiency virus (HIV). Adrenal function abnormality is more common in HIV patients than in the general population. It is important to recognize the condition of adrenal insufficiency, as this adrenal disorder may prove fatal if left untreated. Herein, we report a case of primary adrenal insufficiency in a 37-year-old male patient with acquired immunodeficiency syndrome. The patient complained of fever, general weakness, and fatigue. Impaired adrenal function was noted in the rapid ACTH stimulation test. After steroid supplementation, the patient's symptoms were improved. Therefore, HIV care physicians should ascertain adrenal dysfunction in HIV patients when they complain of fever and general weakness.
-
Citations
Citations to this article as recorded by- A Case Report of Adrenal Insufficiency Treated with Korean Medicine
Young-ji Kim, Jung-yeon Kwon, Ho-yeon Go, Kyung-hwan Kong
The Journal of Internal Korean Medicine.2017; 38(5): 583. CrossRef
- A Case Report of Adrenal Insufficiency Treated with Korean Medicine

- A Case of Adrenocortical Carcinoma Secreting Cortisol, Androgen and Aldosterone.
- Jae Ho Choi, Ye Ri So, Yu Chul Hwang, In Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung, Seung Ae Yang
- Endocrinol Metab. 2011;26(3):239-242. Published online September 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.3.239
- 2,095 View
- 30 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Primary adrenocortical carcinoma is a rare tumor, and is characterized by a peri-tumor mass effect and hormone excess signs. Adrenocortical carcinoma most commonly secretes cortisol, but tumors that secrete other adrenal hormones (aldosterone, androgen) are rare. Herein, we report the case of a 70-year-old woman with cortisol, androgen, and aldosterone-secreting adrenal carcinoma. The patient complained of generalized weakness, moon face, and central obesity. On laboratory examination, hypokalemia and metabolic alkalosis was detected. On the hormone test, cortisol, DHEA-S, and aldosterone were all increased. Abdominal CT showed a large right adrenal mass. She underwent right adrenalectomy and the histology revealed the presence of an adrenocortical carcinoma. After adrenalectomy, the patient was treated with hydrocortisone and mitotane.
-
Citations
Citations to this article as recorded by- A Case of Adrenocortical Carcinoma Secreting Cortisol and Aldosterone
Jiyoon Ha, Min Kyung Kim, Yoon Jin Cha, Seung Kyu Kim, Gi Young Yun, Kwangwon Rhee, Joon Seong Park, Eun-Suk Cho, Chul Woo Ahn, Jong Suk Park
Yeungnam University Journal of Medicine.2012; 29(2): 132. CrossRef
- A Case of Adrenocortical Carcinoma Secreting Cortisol and Aldosterone


 KES
KES

 First
First Prev
Prev



